What is esotropia?
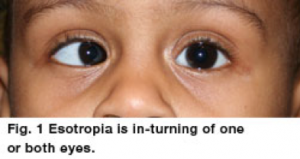
Esotropia is in-turning of one or both eyes [See figure 1]. It may be intermittent or constant and may occur with near fixation, distance fixation, or both. The crossing may occur predominantly with one eye or may alternate between eyes. Esotropia may occur at any age and is the opposite of exotropia (outward eye turn).
Is esotropia ever ‘normal’?
Esotropia in infants less than 20 weeks old frequently resolves spontaneously, especially when the misalignment is intermittent and small in magnitude. However, constant eye crossing at ANY age should be evaluated promptly by a pediatric ophthalmologist. Eye crossing (constant or intermittent) beyond 4 months of age should be evaluated.
What are the different types of esotropia?
Esotropia can be classified by age of onset (congenital/infantile vs. acquired); by frequency (intermittent vs. constant); or by whether it can be treated with glasses (accommodative vs. non-accommodative). For specific information, see infantile esotropia and accommodative esotropia.
Esotropia can also be secondary to other conditions. Poor vision can cause in-turning of an eye. Various neurological conditions (hydrocephalus, stroke, etc.) can cause an eye to turn inward. A number of medical conditions can cause esotropia (thyroid eye disease,Duane syndrome,etc.).
What problems can esotropia cause?
The effect of esotropia on the visual system depends on the frequency/severity of eye crossing and age. Eye crossing affects the ability of the eyes to work together. Older children and adults with a new onset esotropia often experience diplopia (double vision) and or decreased binocular visual field. Children can lose stereopsis (3-D vision) and binocularity (simultaneous use of the eyes) in addition to loss of vision in the crossing eye (amblyopia).
Does esotropia run in families?
Strabismus, or misalignment of the eyes, does run in families. However, affected family members do not necessarily share the same type and/or severity of strabismus. A family history of strabismus is a very good reason for an evaluation by a pediatric ophthalmologist.
Are there conditions that increase the risk of esotropia?
Prematurity, a positive family history, and various neurological and genetic disorders increase the risk of eye misalignment. Also, some systemic disorders cause ocular misalignment (hyperthyroidism, diabetes, etc.).

Do children ever look crossed eyed but actually have straight eyes?
Pseudostrabismus is the appearance of, but not truly misaligned eyes and is usually secondary to the shape of the eyelids and/or nasal bridge [See figure 2]. Any child suspected of having ocular misalignment should have a thorough examination by a pediatric ophthalmologist. Some children can have both pseudostrabismus and actual eye misalignment. Therefore pseudostrabismusdoes not by itself eliminate the possibility of true eye crossing.
How does a Pediatric Ophthalmologist evaluate a child with suspected esotropia?
After taking a careful history, the physician assesses the visual acuity in a manner appropriate for age. A key component is to determine whether the acuity is equal in each eye or if one eye is stronger than the other. Ocular misalignment, if detected, is quantified. The general health of the eye, as well as the refractive state of the eye (ie. farsightedness, nearsightedness, astigmatism) is assessed.
What are the treatment options for esotropia?
Management of esotropia is based on a number of factors. The overriding principles are:
- Re-establishment of ocular alignment
• Maximization of binocular vision
• Relief of diplopia
•Treatment of associated amblyopia
Treatment modalities used to realign the eyes include spectacles (sometimes with prism or bifocal), strabismus surgery (eye muscle surgery), and botulinum toxin (less frequently utilized).
Credits: Journal of American Association for Pediatric Ophthalmology and Strabismus